The 2003 Monkeypox Outbreak Explained
In 2003, the United States experienced an outbreak of a small-pox-like disease endemic to Africa called monkeypox after a handful of Midwesterners were exposed to imported African rodents from Ghana. In 2022, USA Today reported that the same virus was spreading around the world — even among people that had never been to Africa or been in contact with African animals or anyone that had traveled to the continent. In light of the COVID-19 crisis that swept across the world in 2020, there are fears that the global outbreak could trigger another wave of lockdowns (via BBC).
Fortunately, it is not the first time the United States has dealt with this virus. The 2003 outbreak shows that monkeypox — which does not usually transmit easily — can be contained with simple hygiene measures in health facilities and import-export regulations. Here is the story of the 2003 outbreak and how it informs the situation that we face today.
What is monkeypox
The popular fear of monkeypox comes in part from its taxonomic categorization. According to the CDC, the virus that causes monkeypox is part of the Orthopoxvirus genus. As noted in another CDC article, this group of viruses includes the deadly smallpox virus, which is considered eradicated today.
The monkeypox's precise origins and original reservoirs are unknown. The virus got its name after scientists observed an outbreak among captive monkeys. It did not surface in humans until 1970 in then-Zaire (today the Democratic Republic of the Congo) amid mass vaccination campaigns against smallpox in Central Africa. Since 1970, the virus has been determined to be endemic to Central and West Africa's tropical climates but has generally remained restricted to that area until now.
Generally, monkeypox is not deadly, particularly in healthy people. According to a WHO study from 1997, the death rate is anywhere from 1% to 10%, with 3% being the most cited figure. However, some of these likely occurred among malnourished people and very young children, who are most vulnerable to infection (via WHO). This would help explain higher death rates in Africa against the non-existent death rates in the American outbreak.
Symptoms and progression
The progression of monkeypox is similar to that of smallpox, with the exception of the latter's 30% death rate. Per the WHO fact sheet on the disease, the incubation period following exposure is around 5 to 21 days, with two weeks being the most typical. Initially, the symptoms are fairly unremarkable. Patients suffer from typical malaise, fever, lethargy, and muscle aches, similar to the symptoms of other poxviruses. Monkeypox, however, also causes lymphadenopathy (swollen lymph nodes) that allows doctors to narrow down the culprits. The most telling symptom of infection is the characteristic rash that develops a few days into infection. This rash initially starts out as just a rash but then progresses into raised bumps and eventually pustules (pus-filled blisters). The rash can affect the whole body but is typically present on the face, arms, hands, and occasionally genitalia.
Despite the grotesque symptoms of the disease, it is not particularly deadly to healthy individuals. It generally resolves within a month in healthy individuals but can cause complications in immunocompromised individuals, young children, or people with underlying health conditions. Among these are opportunistic secondary infections and encephalitis.
The '97 Congolese outbreak
When the 2003 outbreak surfaced, there was some surprise. As the CDC notes, it was the first time the virus had been detected outside of Africa. Before that, all the outbreaks had occurred in Africa. The most recent outbreak before '03 took place in '97 in the Democratic Republic of the Congo. According to a 1997 CDC report, a joint CDC-WHO investigation identified 92 cases of suspected monkeypox in the DRC's Kasai Oriental region. The number soon grew to 511 cases by the end of 1997. Generally, the death rate in the largest case cluster was among children between 4 and 8 years of age, with a death rate of 1.5% out of 344 cases.
The higher death rate is likely explainable not by the deadliness of the virus but by the context of the outbreak. The outbreak coincided with the First Congo War (via Eastern Congo Initiative), suggesting that the privations of war (e.g., malnutrition) played a role. More notably, however, was the presence of secondary infections. In plain English, this meant that some of the patients had acquired the illness through human-to-human transmission, perhaps through respiratory droplets or contact with the pustules. Per the New Jersey Department of Agriculture, the transmission rate in the Congo outbreak may have been as high as 73% (meaning that 73% of people acquired it from another person). Nevertheless, the outbreak was relatively self-contained, perhaps due to acquired immunity from smallpox vaccination, and it passed under the radar until the American outbreak in 2003.
The 2003 Midwest outbreak
The 2003 outbreak's "patient zero" was a child. According to The Pediatric Infectious Disease Journal, a girl was taken to the hospital with a fever, fatigue, aches, and some other non-specific symptoms. However, it turned out that her parents had purchased a prairie dog from a Chicago flea market, and it died not too long after purchase, along with two other prairie dogs the family kept as pets. In the intervening period, however, the girl had been in contact with the saliva of the Chicago prairie dog. By the time she was admitted, she had already started developing a rash.
Initially, doctors and nurses were hesitant to treat the child because they feared that they were dealing with smallpox — a disease that the United States had stopped vaccinating against since its official eradication in 1980 (via Midland Daily News). However, the girl improved within four days of admission following treatment of the symptoms, making it clear that they were dealing with a related but milder disease. As it turned out, the girl had acquired the monkeypox virus from the prairie dog the family purchased in Chicago and got sick after contact with the animal's saliva. Altogether, there ended up being 47 total cases (via The Journal of Infectious Diseases) in the Midwestern states of Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin.
The Midwest origins
As mentioned earlier, monkeypox was not a disease that would have been expected in the United States. So how did it arrive in the western hemisphere? The girl that first got the disease got it from a prairie dog. But the family's other two pets were healthy until the third sick prairie dog was introduced. Knowing the virus' African pedigree, the CDC's attention turned to a shipment of approximately 800 African rodents imported to Texas from Ghana.
Per a 2003 CDC report, the agency used animal tracebacks to identify the original source of the infections. As it turned out, the prairie dog that infected the girl had been placed in the same container as a handful of African rodents that were distributed to the six Midwestern states that saw cases (in addition to several other states where there was not an outbreak). According to the University of Minnesota, six of these animals were responsible for the outbreak. Then, as the AP reported (reproduced in the Midland Daily News), the animals infected a handful of other pets, including a rabbit, the aforementioned prairie dogs, and other small pets that were sold in pet stores. However, it turned out that the outbreak — which was confined to relatively few people — could easily be controlled, especially in a developed, well-nourished country such as the United States.
The response
The response was fairly straightforward. According to the University of Minnesota, the first step was to euthanize the infected African animals. Any pets that had been exposed were then quarantined. If they tested negative for the virus after six weeks, they were let go. Otherwise, they were euthanized too. Per the Midland Daily News, there was also the fear that pet owners would release potentially-infected animals into the wild, allowing monkeypox to spread to wildlife and make it endemic to North America, so pet owners were ordered not to do this. In the end, no infected animals were released into the wild, as far as any agency was aware.
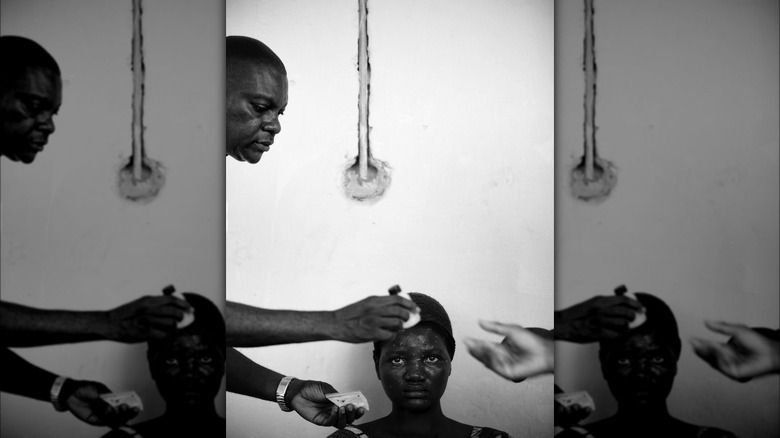
Among infected people (per the CDC), only two patients — both children — had any severe illness, and both of them recovered without any complications. According to the Midland Daily News, the hospitals simply adopted the standard precautionary measures — sterilized dressing, hand-washing and sanitizing, and thoroughly sterilizing uniforms after shifts. No one died, and the outbreak died down as soon as the animals were euthanized and the patients recovered. The Midland Daily News attributed the lack of deaths to the high standard of American healthcare as well as the high standard of living in the United States that allowed patients to be well-fed and healthy. But to ensure that complications did not develop, the patients were vaccinated against smallpox as a precautionary measure.
Transmission
What's interesting about the 2003 outbreak is that there was not one single recorded case of human-to-human transmission. In a study by the journal Clinical Infectious Disease, it was found that healthcare workers who did not observe the full battery of precautions never became infected even after having close, prolonged contact with the patients. For some of these employees, it is possible that because they were vaccinated against smallpox, there was little risk of contracting the virus.
Ultimately, per the New Jersey Department of Agriculture, the chief method of transmission between humans and animals would have been through bodily fluids, such as blood or fluid and pus from the lesions that develop from the disease. In this case, simply wearing gloves likely would have been more than enough to protect health care workers, provided they also washed their hands regularly after interacting with the patients. This contrasted starkly with the '97 outbreak in the Democratic Republic of the Congo, where transmission was much higher — up to 73%, according to some estimates. However, the circumstances in Africa were also very different compared to the United States, suggesting that the disease is only a problem among malnourished populations in countries that lack the ability to respond to it quickly.
Further measures
Once the outbreak was over, the CDC focused on ensuring that the virus did not jump to North American wildlife. In conjunction with the FDA, an order was issued banning the importation of six specific genera of African rodents (the ones that had caused the outbreak) into the United States. Specimens already present in the United States could remain, assuming they were healthy. They can still be bred and sold in the United States — it is just illegal to import them from the African continent.
The order covered several loopholes as well. The rodents could not be imported dead or alive and had to have a traceable history. A common practice of getting around import-export bans is to send contraband to a third country and have it re-packaged and shipped from there. Thus, the ban also applied to any African rodents originating in Africa but shipped from other countries — even if they were born outside of Africa.
There were two exceptions to the rule. Educational and scientific institutions were allowed to import the banned genera as long as they were used solely for research purposes, and this exception required written CDC permission. Taxidermized specimens could also be imported if properly disinfected. Per the CDC, the penalties for individual violations amounted to one year in prison, a $100,000 fine per violation, or both. If importation caused an outbreak that resulted in deaths, the fine was doubled on a per-death basis. Guilty organizations faced $200,000 fines per violation, which increased to $500,000 per death (if any).
Comparison to today
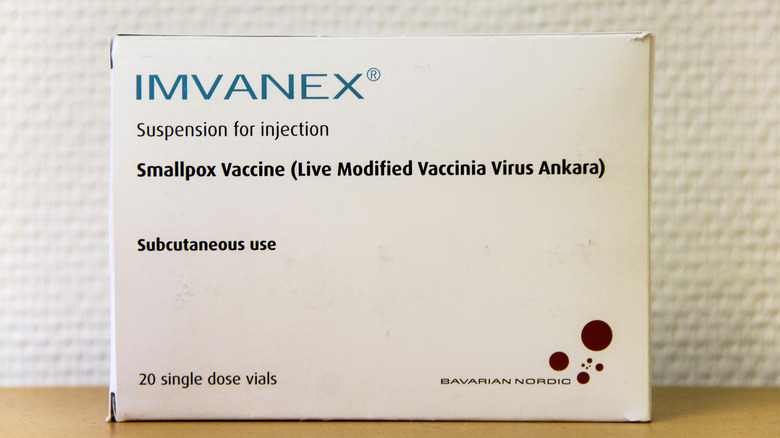
The 2003 monkeypox outbreak is in the news because the virus has allegedly resurfaced on the global scene. As Kent State's Tara Smith noted (via NBC News), given the mildness of the 2003 outbreak, there is little reason to panic. As Time noted, the smallpox and monkeypox vaccines are available and may not even be necessary for most. But the pattern of spread is still concerning. According to CNBC, the uptick in cases has principally affected men who have sex with men, many of whom never visited Africa nor had contact with infected animals, making bodily fluids the likeliest route of transmission. African scientists, meanwhile — who are accustomed to dealing with local outbreaks — have expressed concerns. As quoted in ABC News, the current spread does not mirror previous infection patterns, suggesting that "something new" is happening, per the former head of the Nigerian Academy of Sciences, Oyewale Tomori.
Because of similar concerns during the COVID-19 crisis, there are suggestions that this "something new" may be the modification of the virus through gain of function research. In fact, the Munich Security Conference (via Science Business) war-gamed such an outbreak of a souped-up virus in 2021. The Wuhan Institute of Virology has been accused of performing gain of function research on the virus, but biolabs such as Wuhan are not considered to be the source of the outbreak — at least according to currently-available evidence (via the Spectator).